Two major women’s health organizations, Susan G. Komen for the Cure and Planned Parenthood, battled for women’s respect and donations. Two days later the dust is settling and we’re left to wonder what we should take away from the tangle? Was it about fundraising? Women’s health? Politics? I suggest it is about stigma, specifically abortion stigma that has been deliberately attached to a beloved national institution and household name, Planned Parenthood.
Unsafe abortion’s significant contribution to maternal mortality and morbidity was a critical factor leading to liberalization of Nepal’s restrictive abortion law in 2002. Careful, comprehensive planning among a range of multisectoral stakeholders, led by Nepal’s Ministry of Health and Population, enabled the country subsequently to introduce and scale-up safe abortion services in a remarkably short timeframe. This paper examines factors that contributed to rapid, successful implementation of legal abortion in this mountainous republic, including deliberate attention to the key areas of policy, health system capacity, equipment and supplies, and information dissemination.
At a time when the pool of abortion providers is shrinking and abortion clinics are closing, medical abortion can truly increase women’s access, particularly to those in underserved areas. For legislators who want to end access to abortion under any circumstances, medical abortion is an obvious target.
The new WHO recommendations make it painfully clear that, nearly 40 years after Roe v. Wade, we’re doing everything wrong here. Whether it’s gestational limits, ultrasounds, counseling or human rights, nearly every policy proposed by anti-abortion legislators directly contradicts the new WHO guidelines, which are based on years of consultation and discussion, incorporating scientific evidence and international human rights standards.
Unsafe termination of pregnancy is a major contributor to maternal morbidity and mortality. Task sharing termination of pregnancy services between physicians and mid-level providers, a heterogeneous group of trained healthcare providers, such as nurses, midwives and physician assistants, has become a key strategy to increase access to safe pregnancy termination care.
This study aimed to understand women’s pathways of seeking care for postabortion complications in Madhya Pradesh, India. The study recruited 786 women between July and November 2007.
Despite Zambia’s relatively progressive abortion law, women continue to seek unsafe, illegal abortions. Four domains of abortion attitudes – support for legalization, immorality, rights, and access to services – were measured in 4 communities.
Unsafe abortion is a significant contributor to maternal mortality in Nigeria, and treatment of postabortion complications drains public healthcare resources. Provider estimates of medications, supplies, and staff time spent in 17 public hospitals were used to estimate the per-case and annual costs of postabortion care (PAC) provision in Ogun and Lagos states and the Federal Capital Territory.
To address the knowledge gap that exists in costing unsafe abortion in Ethiopia, estimates were derived of the cost to the health system of providing postabortion care (PAC), based on research conducted in 2008.
Unmet need for family planning is typically calculated for currently married women, but excluding husbands may result in misleading estimates of couples’ unmet need. This study builds on previous work and proposes a method of calculating couples’ unmet need for family planning based on spouses’ independent fertility intentions.
Because Brazilian law only permits abortion in cases of rape, fetal anencephaly, or risk to life, in 2012 the country’s Ministry of Health reported only 1,626 legal abortions in a nation with 203 million people. However, an estimated one million Brazilian women have abortions every year. Many of those women, particularly those without the financial or social resources to see a well-trained, willing provider, run a huge legal risk when they decide to end an unwanted pregnancy. The physical consequences also can be devastating.
This study assesed the severity of abortion complications in Malawi and determined associated risk factors. Between July 20 and September 13, 2009, a cross-sectional survey was conducted at 166 facilities providing postabortion care services.
Certainly, sharing abortion stories can be a powerful act and may reduce self-stigma. But I fear that it distracts from the structural inequalities of race, poverty, age, and education by placing too much emphasis on the individual. And I worry that it lets our politicians and policymakers off the hook.
Guidance for postabortion care (PAC) is established for the first trimester but limited in the second trimester. Objective: To establish evidence-based recommendations for PAC in the second trimester. Conclusion: Misoprostol with or without mifepristone is an effective treatment for second-trimester PAC. The minimum misoprostol dose is 200 μg vaginally, sublingually, or buccally every 6–12 hours.
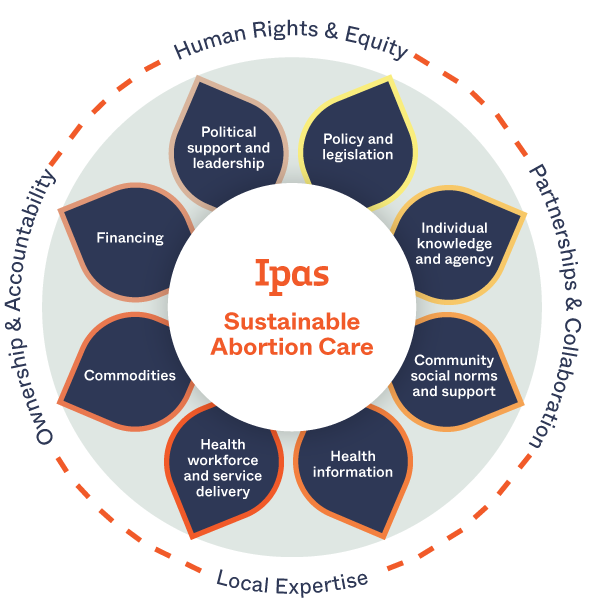
A comprehensive structured program design, collaboration between the MOH and Ipas, and provider dedication enabled successful introduction of second-trimester abortion services in major regions/states of Ethiopia. A focus on second- trimester medical abortion allows for rapid service introduction without extensive changes to facilities, equipment, or staffing as the needs are similar to obstetric care.
The African Commission on Human and Peoples’ Rights recently adopted General Comment No 2 to interpret provisions of Article 14 of the Protocol to the African Charter on the Rights Women.
This study describes postabortion complication severity and associated factors in Kenya. A nationally representative sample of 326 health facilities was included in the survey. Data were collected from 2,625 women presenting with abortion complications.