The Zika virus epidemic has reached more than 20 countries in the Americas and is the potential cause, with circumstantial evidence, for thousands of cases of microcephaly, in addition to other neurological consequences. This calls for a public debate on women’s right to interrupt the pregnancy if they so desire, as an issue of reproductive social justice.
Abortion has been legal in Nepal since 2002, and post-abortion care has been successfully integrated into hospitals. But that does not mean that women can easily obtain safe abortion services. The barriers are many, and women are often stigmatized for the decision to end a pregnancy.
It is time for accountability and for concerted action. Millions of women in Brazil and throughout Latin America have already been living with constrained choices regarding their reproductive lives—Zika has further aggravated their situations.
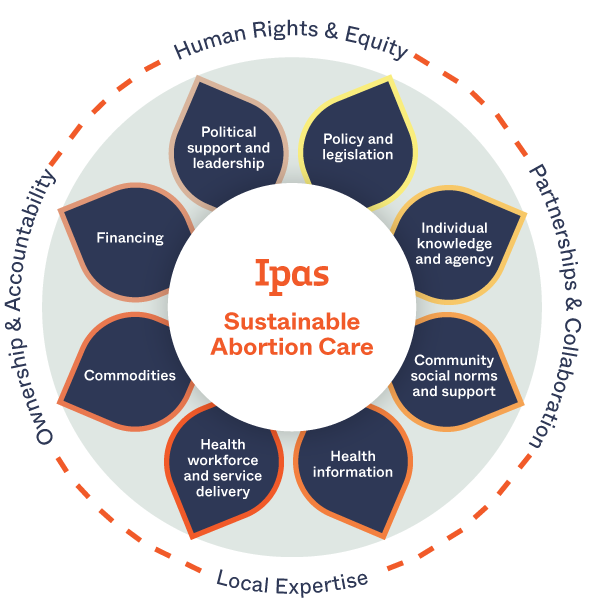
Contraception is an essential element of high-quality abortion care. However, women seeking abortion often leave health facilities without receiving contraceptive counselling or methods, increasing their risk of unintended pregnancy. This paper describes contraceptive uptake in 319,385 women seeking abortion in 2,326 public-sector health facilities in eight African and Asian countries. Ministries of Health integrated contraceptive and abortion services, with technical assistance from Ipas. Overall, postabortion contraceptive uptake was 73 percent. The findings demonstrate high contraceptive uptake when it is delivered at the time of the abortion, a wide range of contraceptive commodities is available, and ongoing monitoring of services occurs.
The presence of religious conservatives with an anti-woman, anti-gay, anti-trans agenda at the OAS is not new. But it is of increasing concern as they continue agitating to dismantle human rights while scenes of unprecedented violence play out across the world…As Orlando demonstrates, any setback to human rights, as designed by these groups, will only lead to more violence.
This study compared levels of abortion stigma in regions with high and low incidence of unsafe abortion in Kenya to explore whether abortion-related stigma is associated with incidence of unsafe abortion. Respondents from a county with higher incidence of unsafe abortion reported higher stigma scores. Age, marital status, type of abortion service, and socioeconomic status were all significantly associated with stigmatizing attitudes.
This study sought to explore abortion-related stigma at the community level as a barrier to women realizing their right to a safe, legal abortion. It found that abortion-related stigma plays a major role in a woman’s decision on whether to have a safe or unsafe abortion. Young unmarried women, in particular, bore the brunt of being stigmatized.
The importance of South Africa as a model for reproductive self-determination in Africa cannot be underestimated. Abortion has been legal since 1996, and the country has some of the most developed government systems for the provision of abortion care on the continent. Yet in the same way opponents of abortion in the United States have whittled away at access with increased bureaucracy, South Africa faces similar assaults that leave women without safe care and threaten to turn back achievements made during the past 16 years. This article explores the history of the law, subsequent legal challenges, and new threats to women’s access to abortion services, including service delivery issues that may influence the future of public health in the country.
The stigma that often surrounds abortion and anyone associated with it—women, providers, pharmacists and advocates—contributes to abortion’s social, medical and legal marginalization. At Ipas, we know that stigmatizing abortion is inherently harmful to women’s health — preventing them from getting the care they deserve.
More than half the population supports gay marriage and families. So when will abortion and women’s rights to reproductive self-determination be a cultural norm?
This study evaluates the implementation of misoprostol for postabortion care (MPAC) in two African countries, Kenya and Uganda. The Ministries of Health, local health centers and hospitals, and NGO staff developed evidence-based service delivery protocols to introduce MPAC in selected facilities; implementation extended from January 2009 to October 2010. RESULTS: In both countries, MPAC was easy to use, and freed up provider time and health facility resources traditionally necessary for provision of PAC with uterine aspiration. On-going support of providers following training ensured high quality of care. Providers perceived that many women preferred MPAC, as they avoided instrumentation of the uterus, hospital admission, cost, and stigma associated with abortion.
This paper reports results from a nationally representative health facility study conducted in Ethiopia in 2008. It provides the first national snapshot to measure changes in a dynamic abortion care environment.
Blog post contributed by Dr. Osur to the Women Deliver website in preparation for the 2013 conference in Kuala Lumpur. Ipas is a sponsor of Women Deliver.
Beatriz, a 22-year-old Salvadoran mother with lupus and kidney failure, is pregnant with an anencephalic fetus but continues to be denied a therapeutic abortion by the restrictive law in her country.

Lessons learned from integration of postabortion care, menstrual regulation, and family planning services in Bangladesh. This study recommended working toward improved post-procedure contraception delivery and evidence-based appropriate technology use for all procedures by improving collaboration and integration between Bangladesh’s Directorate General of Health Services (DGHS) and Directorate General of Family Planning (DGFP).
Understanding what factors influence the receipt of postabortion contraception can help improve comprehensive abortion care services. The abortion visit is an ideal time to reach women at the highest risk of unintended pregnancy with the most effective contraceptive methods. The objectives of this study were to estimate the relationship between the type of abortion provider (consultant physician, house officer, or midwife) and two separate outcomes: (1) the likelihood of adopting postabortion contraception; (2) postabortion contraceptors’ likelihood of receiving a long-acting and permanent versus a short-acting contraceptive method.